Tiny, maggot-like bot could kill hard-to-reach brain tumors
A light bulb goes off when a neurosurgeon sees plastic surgeons use sterile maggots to remove dead tissue.
When J. Marc Simard, a neurosurgery professor at the University of Maryland, saw a TV show a few years back with plastic surgeons using sterile maggots to remove dead tissue from a patient, the proverbial light bulb went off.
"Here you had a natural system that recognized bad from good and good from bad," Simard said last week in a press release from the National Institute of Biomedical Imaging and Bioengineering. "The maggots removed all the bad stuff and left all the good stuff alone, and they're really small. I thought, if you had something equivalent to that to remove a brain tumor, that would be an absolute home run."
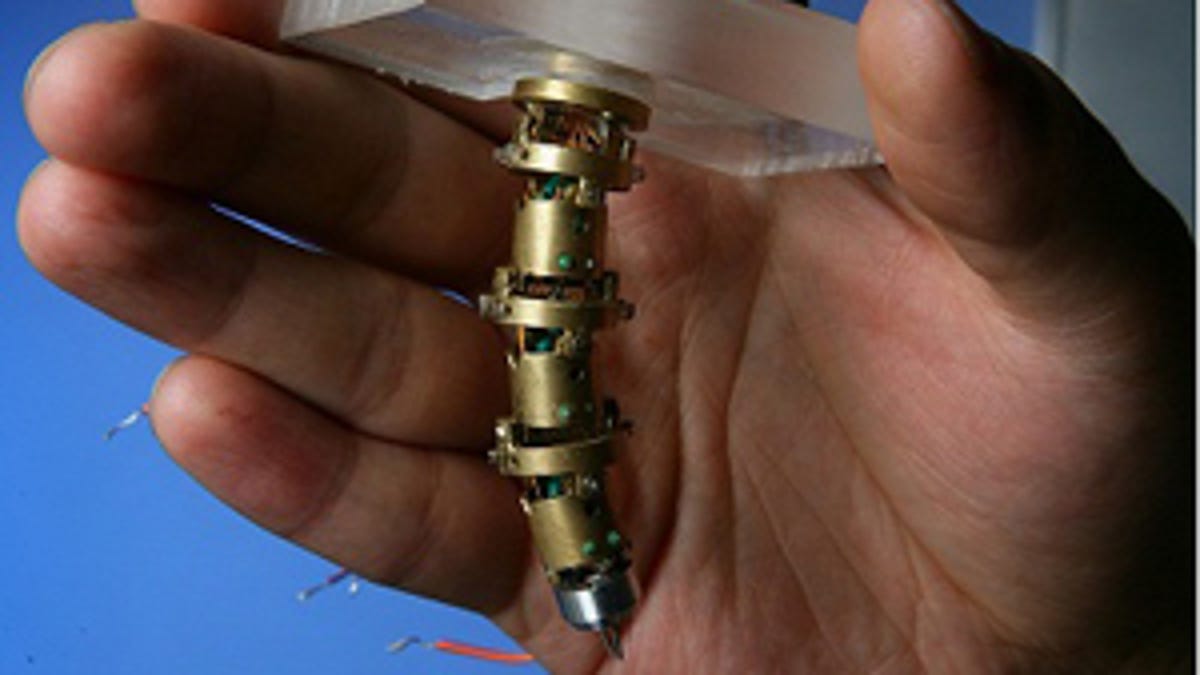
Now four years into development, Simard and his team are working on an intracranial robot prototype that resembles a mechanical fingertip with several joints and, thanks to an electrocautery tool and suction tube on its tip, can heat and destroy tumors and suction out debris. Better yet, it can be remotely controlled by a surgeon while the patient is in an MRI scanner -- providing the surgeon with the best view of the tumors that are hardest to see and reach.
"When we're operating in a conventional way, we get an MRI on a patient before we do the surgery, and we use landmarks that can either be affixed to the scalp or are part of the skull to know where we are within the patient's brain," Simard said. "But when the surgeon gets in there and starts to remove the tumor, the tissues shift around so that now the boundaries that were well-established when everything was in place don't exist anymore, and you're confronted once again with having to distinguish normal brain from tumor. This is very difficult for a surgeon using direct vision, but with MRI, the ability to discriminate tumor from non-tumor is much more powerful."
To make this possible, the surgery itself involves several steps, starting with the insertion of the bot into the brain outside of the scanner, then moving the patient into the scanner and controlling the bot from a different room, then moving the bot deep inside the brain to zap the offending tumor(s), and finally removing the patient from the scanner and the bot from the patient. Even so, the complex approach removes a lot of the guesswork currently involved in this type of nuerosurgery.
Simard's team is not alone on its cusp of a major breakthrough. Scientists at the University of Washington are concurrently working on a scanning fiber endoscope -- for imaging within the narrow bile ducts inside the liver -- to be used during brain surgery as well. A traditional endoscope, which sports a tiny video camera at one end, can produce real-time video during surgery.
Problem is, the thinner the endoscope, the lower the resolution, and endoscopes need to be very thin to reach deeply into the brain. "Right now, with the current state of the art ultrathin endoscopes, I calculate based on the field of view and their resolution that the person looking at that display would see so little as to be classified in the US as legally blind," said Eric Seibel, a professor of mechanical engineering who developed the endoscope.
Fortunately, Seibel has recently been able to retain image quality while whittling the size of the endoscope down to the diameter of a toothpick. His endoscope replaces the video camera with a single optical fiber the width of a human hair that releases white lasers when vibrated at a particular frequency that then shine through a series of lenses to provide a 100-degree field of view.
"It's almost like putting your eyes inside the body so you can see with the wide field view of your human vision," Seibel said.
Both approaches are still early in development and will require extensive clinical investigation before seeing the light of an operating room, but the potential is there for some serious tumor-conquering.

